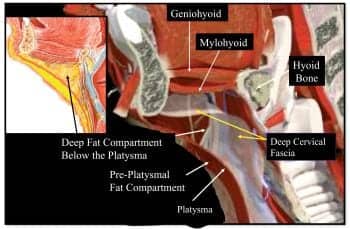
Figure 1. Cross section of the mandible and submental region demonstrates where the two main fatty compartment exist above and below the platysma. Typically, patients with obtuseshaped necks (genetically based) or simply a heavy neck carry the majority of their fat in the compartment deep to the platysmal muscle.
As the demand for esthetic procedures has increased, so has an increased public awareness of the results that can be achieved. Patients frequently request a more defined jawline, removal of excess submental fat, and improvement in submental skin laxity. A variety of procedures are available, but it is important to properly diagnose the patient and select the appropriate procedure in order to obtain maximal results.
Patients that complain of poor neck contour are often shocked when a facelift is the procedure recommended by the surgeon. The patient is often not prepared to undergo a more invasive procedure, but still desires improvement in neck contour.
While a full lower facelift and neck lift remains the gold standard for improvement of the neck and jowls, less invasive procedures—such as liposuction, chin implants, or submentoplasty—may often be used alone or in combination to improve poor neck esthetics.
It is important for the surgeon to recognize the limitations of each procedure and counsel patients appropriately. Fortunately, many patients may be candidates for less invasive procedures that give a desirable result.
NECK EVALUATION
It is important for the surgeon to rule out any pathologic process that could contribute to the patient’s chief complaint of submental (neck) fullness or poor neck contour, such as thyroid disease or salivary gland pathology.
In general, younger patients with good skin tone will be better candidates for liposuction. If the patient has tremendous skin laxity, less dramatic improvement can be achieved with liposuction even if a significant amount of submental (under the chin) fat is present.
Determining the amount of preplatysmal (area above this neck muscle) fat can be done by gently pinching the skin with your fingers. If there is still sufficient fullness with this maneuver, then the patient may also have significant deposits of subplatysmal (deep to this muscle) fat, which cannot be properly addressed with liposuction alone. A submentoplasty should be considered in order to excise the fat under direct vision (Figure 1).
Next, the position of the hyoid bone (found an inch or so above the Adam’s apple) should be noted by palpation. A low, anterior positioned hyoid bone will result in a less than ideal outcome even with diligent surgical technique. Recognizing this prior to the procedure will allow you to discuss the limitations or possible alternatives, such as camouflaging the obtuse chin-neck angle with a chin implant.

Figure 2. Before-and-after of the ideal patient for liposuction of the neck who is typically less than 40 years old, excellent skin and muscle tone (no platysmal banding), along with localized superficial fat.
Signs of an aging neck include jowling and platysmal muscle banding, which is the vertical cords that appear with age. Platysmal banding occurs as a result of a weakened platysmal muscle and is most noticeable in thinner patients. This can be considerably improved by submentoplasty. However, platysmal laxity along with jowl and skin laxity is best treated with a full lower face and neck lift with concurrent submentoplasty to repair or sometimes excise the platysmal muscle.
Another important factor to consider is submandibular (salivary) gland ptosis. This occurs when the submandibular gland is visible as a small chestnut-sized mass in the neck several centimeters below the angle of the mandible. If left unrecognized, the esthetic result will be less than satisfactory with traditional liposuction and submentoplasty. In fact, aggressive liposuction may cause the patient to recognize submandibular gland ptosis that they did not notice preoperatively.
Partial submandibular gland removal is an option for a very select few with this problem, but many surgeons find this procedure challenging via a small submental crease incision. Informing the patient of the limitations is likely better than attempting a procedure you are not comfortable performing.
LIPOSUCTION
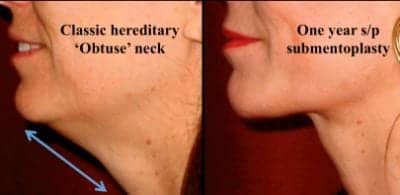
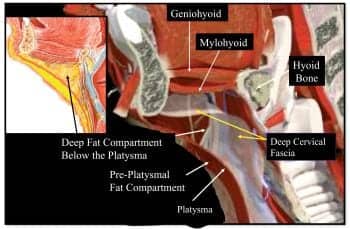
Figure 3. A classic patient with an obtuse-shaped neck (genetic origin) that presents with the majority of their fat in the compartment deep to the platysmal muscle. The patient shown is a 44-year-old before and 1 year following an isolated submentoplasty using anterior plication after back cuts and deep fat direct excision, but no liposuction or skin excision.
The ideal candidate for liposuction is usually a patient less than 40 years of age with good skin tone and favorable muscle and bone structure (Figure 2).
Minor platysmal banding could be treated with botulinum toxin type A injections to the platysma in conjunction with liposuction. However, significant platysmal banding or skin laxity should be treated with submentoplasty and possible facelift.
The technique for neck and lower facial liposuction has evolved. Previously, surgeons used large, spatulated cannulas to extract as much fat as possible. Initial results were often good, but over time patients developed a skeletonized appearance of the neck. Also, it was easy to have uneven fat removal and develop a lumpy appearance.
Today, the trend is to use microcannulas that are 1 mm to 1.5 mm in diameter. The goal for cervicofacial liposuction is to resculpt the neck to improve the contour, not to remove all the fat. Uniform fat removal is critical without excessive dermal injury. As with any liposuction, cannula movement from more than one direction helps maintain a smooth contour.

Figure 4. A 60-year-old female before and 7 1/2 years after an isolated submentoplasty with no skin excision and a small chin implant. The patient was a good candidate for a submentoplasty versus liposuction because of the platysmal laxity and moderate deep fat present below the platysma, yet relatively good skin tone and no desire for a traditional facelift.
While laser and ultrasonic liposuction may prove to better shrink skin, surgeons should still use caution in using these modalities alone when skin or platysmal laxity exist in the neck. Early results following any liposuction will often not show contour irregularities or what will happen to the skin and muscle bands 6 months or years later.
Patients are instructed preoperatively that the expected outcome of fat removal is that the skin will shrink into a new contour. It is important to warn the patient that if excess skin laxity develops after the procedure, then additional rejuvenation may be required.
SUBMENTOPLASTY
A submentoplasty may be required for patients with platysmal banding or subplatysmal fat deposits in the neck. Many times this is done in conjunction with a facelift. If there is no significant jowling or if the patient does not desire a more invasive procedure, submentoplasty in isolation may be considered if adequate skin tone in the neck exists (Figure 3).
Often, a chin implant can be placed simultaneously to further enhance the neck contour by lengthening the horizontal neck from the chin point to the hyoid bone (Figure 4).
The technique consists of a 3-cm to 4-cm incision made in the submental crease if no chin implant is planned; or, the same incision length made a few millimeters posterior to the crease if planning a simultaneous implant, so that the scar remains hidden after forward stretch.
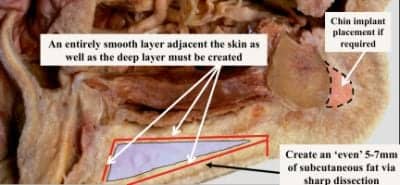
Figure 5. Cross section of the mandible and submental region demonstrates where the two main fatty compartment exist above and below the platysma. Typically, patients with “obtuse”-shaped necks (genetically based) or purely a heavy neck carry the majority of their fat in the compartment deep to the platysmal muscle.
The skin is then elevated in the subcutaneous plane, leaving a thin, smooth continuous layer of subcutaneous fat attached (Figure 5). No liposuction is performed prior to skin elevation to avoid irregularities, damage, or exposure to underlying dermis.
Open liposuction may be performed following skin elevation to “clean” off residual preplatysmal fat from the platysmal surface, to clearly see the quality and shape of the muscle prior to direct treatment.
Platysmal edges can be sewn together (plicated) at the midline to repair any midline dehiscence, but most often results are improved by first removing excess midline redundant platysma and excess subplatysmal fat.
Subplatysmal fat resection is usually necessary with heavy necks. Care must be taken to do this evenly. The subplatysmal fat can be directly excised with scissors or cautery using a lighted retractor. The platysma muscle may require partial resection if it is too thin to adequately hold midline sutures.

Figure 7. There are two foremost situations demonstrated here that may warrant a submentoplasty:
1) To enhance facelift results in patients with major submental skin or muscle laxity and subplatysmal fat excess.
2) As an isolated procedure in patients with adequate skin tone that need more than liposuction due to deep fat and platysmal redundancy.
Uniform removal of deep fat must be performed laterally as well as centrally to avoid a “cobra neck” deformity. This midline depression can be seen after excessive fat removal from the midline or inadequate platysmal treatment. Elevation of the lateral platysma in the neck gives access to the often-neglected deep fat over the submandibular gland.
Deep, lateral elevation of the platysma with cautery and a lighted retractor can be performed to prevent relapse of platysmal bands from postoperative dehiscence of midline sutures (Figure 6).
If muscle plication is to be performed, a very clean and thick deep plane flap should be elevated and advanced under very little tension, typically closed in a double layer from the chin to the hyoid.
While the plication is necessary in the average or thin patient to avoid a skeletonized appearance, it is often not necessary in an obese neck patient and can even compromise the result.
In special situations, where there is plenty of subcutaneous fat on a heavy neck, the majority of the anterior platysma can be resected along with the deep fat. With special care to create a uniform layer of deep fat and neck musculature in the very obese neck, resection of the platysma and subplatysmal fat will often lead to a longer-lasting and maximized result in this more difficult patient population. Though challenging through a small incision, this technique can give wonderful results if diligently performed.
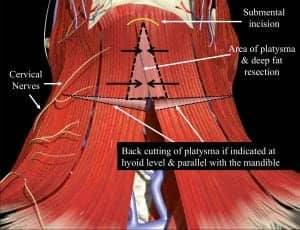
Figure 6. The anterior neck diagram demonstrates where the classic triangular area of platysma is classically excised along with excessive subplatysmal fat. If desired, horizontal transection through the platysma at the level of the hyoid can also be performed to allow medialization platysmal flaps. Horizontal cuts, if used, must remain parallel and at least 2 cm below the mandible to avoid marginal mandibular nerve injury.
SUBMENTOPLASTY WITH FACELIFT
Some surgeons feel that a submentoplasty is almost always a necessity when simultaneously performing a facelift, although many facelift surgeons do not necessarily perform it.
There are two prevalent reasons for not performing a simultaneous submentoplasty in conjunction with a facelift. First, some believe it is not worth the time because the pulling back of deeper tissues by the ear improves the front neck tissues. While this may be true for some necks initially, it inevitably leads to relapse of tissue laxity 4 to 6 months following the facelift.
Second, midline platysmal plication may compromise elevation you could otherwise achieve in the jowl region because of a competing pull in opposite directions.
The goal in any cosmetic rejuvenation procedure is a more youthful appearance that is both natural and long-lasting. Combining an anterior platysmalplasty with a facelift is usually necessary to achieve maximum results when significant lower facial skin laxity exists.
In general, if there is significant subplatysmal fat and/or submental skin laxity with platysmal bands, along with jowling, then a lower facelift with submentoplasty is required. Facelifting without a submentoplasty is usually reserved for relatively thin patients with jowling and minimal submental laxity of skin or muscle.
PARTIAL SUBMANDIBULAR (SALIVARY) GLAND RESECTION
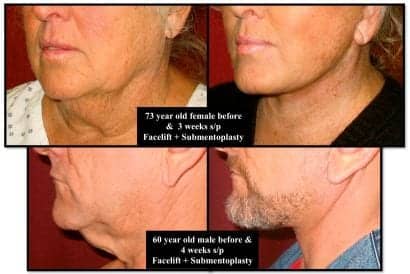
Figure 8. Two patients shown demonstrate classic lower face and neck lifts combined with aggressive submentoplasty. The 73-year-old female had extremely heavy subplatysmal fat that was excised along with excision of a large portion of redundant platysma without plication. The 60-year-old male shown has minimal fat but extreme skin and platysmal laxity requiring anterior platysmal resection along with lateral undermining and anterior plication.
This technique is used principally for patients who have had previous neck liposuction or facelifting and now notice their submandibular glands bulging for the first time just below their jawline on either side.
Typically, the patient worries because they are unsure of the etiology of their recently noticed neck bulge despite tight skin. An astute surgeon may occasionally diagnose enlarged or ptotic submandibular glands prior to an initial neck surgery. Unfortunately, it is usually seen as a side effect subsequent to a cosmetic procedure. Over-resection of fat may contribute to the problem.
The options for repair are limited. Simply reassuring the patient after a procedure may be adequate, especially if it was discussed as a risk during the preoperative visit. Surgical treatments are available, but have a mixed history of success combined with a higher than average complication rate even with experienced surgeons.
My particular technique has been used for more than 7 years in patients with either primary or secondary submandibular gland fullness (Figure 9).
The procedure is performed solely through a submental crease incision beneath the chin. The platysma muscle is elevated off the gland on each side immediately inferior to the gland. Excellent visualization is critical along with an expert knowledge of the local anatomy to perform this procedure through such a small incision.
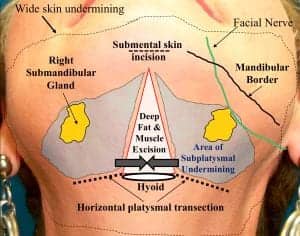
Figure 9. The diagram demonstrates the extensive submental dissection required to partially excise excess submandibular gland tissue during a submentoplasty. It is challenging to approach the gland from below through a 4-cm submental incision above. The use of a lighted retractor is required along with meticulous bloodless dissection
The excess gland is amputated in an inferior-to-superior direction, with cautery and lighted retraction. This is followed by closure of the cervical fascia over the raw residual gland to help prevent a sialocele. The procedure is for experienced surgeons and has a high learning curve because of the instrumentation required in the limited space. Results may be worth the added risk for very select patients (Figure 10).
FACIAL IMPLANTS AND OTHER NECK TREATMENTS
Adding a chin implant or occasionally mandibular angle implants can dramatically improve the neck contour by strengthening the mandibular border.
A chin implant further lengthens the upper neck to improve a chin-neck angle in someone who has microgenia. In the right patient, a chin implant can make a major difference in the end result.
COMPLICATIONS
In general, complications following submentoplasty closely resemble complications following neck liposuction alone, such as dermal injury with abnormal postoperative swelling, skin irregularities, prolonged swelling, seromas, hematomas, sialoceles, transient and permanent injury of nerves, and postinflammatory skin color changes.
Hematoma occurs in approximately 3% of facelift patients and usually occurs within the first 24 hours. It occurs most often a few hours after the anesthetic wears off. The patient experiences pain and has an increase in blood pressure. Early treatment is critical. Without adequate and early treatment, hematomas can result in hyperpigmentation and rippling of the skin secondary to subdermal scarring. Swelling will also be much worse.

Figure 10. The photos demonstrate the appearance of a patient preop with bilateral bulging submandibular glands that would likely look more obvious following a standard facelift. She underwent a facelift with submentoplasty and simultaneous partial excision of excess submandibular gland.
Skin slough (or skin loss) is generally not a problem in patients undergoing an isolated submentoplasty, but could be a potential dreadful sequela following an untreated expanding hematoma. Aggressive and early management is needed along with frequent and close follow-up appointments. This complication is much more common with patients who smoke and have facelift surgery.
Another unfortunate complication is adhesion of the platysma or digastric muscles to the overlying skin when excess fat has been removed through liposuction or surgical technique. This can result in a rippled or uneven appearance to the skin.
Also, over-resection of deep tissues may produce an unsightly, “skeletonized” appearance that is also difficult to treat and should be avoided if at all possible.
You can prevent this by leaving adequate fat on the skin surface, as well as meticulous removal of only the excessive fat in the deeper layers.
CONCLUSION
Selecting the best technique for changing neck contour is vital to obtain the best result possible.
Angelo Cuzalina, MD, DDS, is in private practice in Tulsa, Okla, and is the current president of the American Academy of Cosmetic Surgery. He can be reached at www.tulsasurgicalarts.com.
FURTHER READING:
- Cuzalina LA, Koehler J: Submentoplasty and facial liposuction. Oral Maxillofac Surg Clin North Am. 2005;17(1):85-98.
- Connell BF. Neck contour deformities: The art, engineering, anatomic diagnosis, architectural planning, and aesthetics of surgical correction. Clin Plast Surg. 1987;14:683.
- Feldman JJ. Corset platysmaplasty. Plast Reconstr Surg. 1990;333-343.
- Klein JA. The tumescent technique for liposuction surgery. Am J Cosmetic Surg. 1987;4:263-267.
- Coutiss E. Suction lipectomy of the neck. Plast Reconstruc Surg. 1985;76:882.
- Hodgkinson DJ. Clinical applications of radiofrequency: nonsurgical skin tightening (Thermage). Clin Plast Surg. 2009;36:2;261-268.
- Goldman A. Laser-assisted liposuction. Clin Plast Surg. 2009;36(2):241-253.
- Matilde M. New indications for Botulinum Toxin A in cosmetic: mouth and neck. Plast Reconstr Surg. 2003;112:75S-85S.
- Gryskiewicz J. Submental suction-assisted lipectomy without platysmaplasty: pushing the skin envelope to avoid a face lift for unsuitable candidates. Plast Reconstr Surg. 2003;112:1393-1405.
- Little JW. In treatment of the full obtuse neck (panel discussion). Aesthetic Surg J. 2005;25:387.