You can’t help but notice it everywhere, whether you’re “people watching” in a shopping mall or watching the evening news. Many people in the United States are obese, and the problem is getting worse.
Not surprisingly, billions of dollars are spent annually in search of weight-loss solutions, from personal trainers to organizations such as Weight Watchers.
Today, one of the most popular answers is bariatric surgery. More people are opting for the surgical alternative, with its consistent track record of success.
Concurrent with this increase in weight-loss surgery is an unprecedented increase in demand for body-contouring procedures performed by plastic surgeons.
Within the weight-loss population, a growing absolute number and overall percentage of male patients are seeking aesthetic surgery.
In this unique group of people, men seeking surgical body-contouring procedures comprise around 10% of the overall population.
Body-contouring surgery produces dramatic outcomes and consistently high levels of patient and physician satisfaction.
WEIGHT LOSS AND THE MALE BODY
As men gain weight, the skin is all too accommodating in expanding to meet the body’s growing size.
As the pounds are shed, the skin is not as resilient. After significant weight loss, patients are left with widely varying amounts of excess skin and associated deformity.
Deformities in men are similar to what women experience in the arms and legs, but are much different in the central trunk and chest.
In the male abdomen, as weight loss is not compounded by the changes of pregnancy, rectus diastasis is not as great a contributing factor as in women. Additionally, posterior fibrous tissue attachments are stronger; the end result is less buttock ptosis.
In the chest, significant weight loss can result in minimal deformity to significant gynecomastia. The approaches to treatment vary according to the degree of residual tissue and nipple ptosis. In my opinion, addressing the male chest is the most challenging aspect of weight-loss patient care.
I have found weight-loss patients to be among the most educated of the prospective patients seeking plastic surgery. Most have been watching their bodies change for months or years and have come to grips with the fact that plastic surgery is a necessity.
They scour the Internet and participate in local and national support groups. They have a thirst for information, and I satisfy their need by educating them as fully as possible prior to surgery.
The process begins before our first meeting. A Web site, Afterobesity.com, covers many topics from getting started in weight loss to the differences in surgical procedures. Designed to be a comprehensive resource, it supplies information about nutrition, surgical preparation, insurance considerations, and important resources locally and nationally.
Many patients come to their consultation well informed, which makes the first meeting all the more valuable.
Prior to the consultation, we send an information package to our prospective patients with detailed information about our practice as well as specific information about weight-loss-related surgeries.
 |
 |
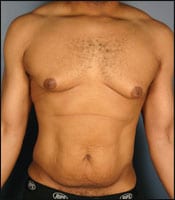
| Figure 1. Almost all patients who have achieved significant weight loss require multiple areas of body treatment. Most often, the procedures are done in a staged fashion. | |
We encourage patients to bring in their spouse, significant other, or whoever will serve as their postoperative support system.
The initial consultations are conducted in a family room type of setting, which to some degree reduces the anxiety associated with the appointment.
We also have masculine, bathrobe-style gowns that can be worn during the examination—this kind of detail shows commitment and sensitivity toward male patients. Examinations are chaperoned in such a way to ensure privacy. During the consultation, I convey the following main points:
- Body-contouring surgery is complex and often involves multiple stages.
- Patients need to participate in making the many decisions involved to optimize results.
- Medical considerations need to be addressed, and a thorough medical evaluation is mandatory.
- Risks exist and should not be taken lightly.
- Insurance authorization will take time and patience.
- The “whole person” concept needs to be embraced to ensure the best patient outcome.
- Weight-loss surgery is essentially a trade of excess skin and fat for scars.
At the conclusion of our consultation, the patient and I develop a plan of care to include surgical treatment, stages (if necessary), and expected outcome. We also discuss the limitations of surgery based on presenting condition.
PREOPERATIVE EVALUATION
Physical demands placed on the overweight body can cause serious medical problems. It is well known that obesity contributes to high blood pressure, diabetes mellitus, muscle and joint pain, and depression. After significant weight loss, amelioration of these conditions is the norm.
Although patients may still require medications, often their general health is outstanding. Nevertheless, occasionally I encounter a few problems.
After bariatric surgery, food intake is obviously altered. The resulting decrease in calorie intake and the concomitant decrease in protein may result in poor wound healing, anemia, and possibly impaired clotting mechanisms.
Prior to plastic surgery, it is important that you complete simple lab tests in order to ensure that the liver and kidneys function properly, blood clotting is appropriate, and cell counts are within normal ranges.
Also, prior to reconstructive surgery it is vital that protein intake is optimized. We often recommend Boost, Ensure, or other supplements that increase protein and promote wound healing—that is, if patients can tolerate these products without experiencing the dumping syndrome.
In addition, patients should have eliminated empty calories from their diet.
Finally, depending on the patient’s age and health status, more extensive testing may be involved, including an EKG, stress tests, or more comprehensive laboratory evaluations. The specific set of tests is determined on a patient-to-patient basis.
 |
 |
| Figure 2. At the time of the body lift, I also perform medial thigh liposuction to get this area to contract as much as possible, especially in patients who are considering medial thigh lifts in the future. | |
Almost all patients who have achieved significant weight loss require multiple areas of body treatment. Most often, the procedures are done in a staged fashion, although occasionally they can be completed in a single operative session.
The use of both novel and tried-and-true techniques and medications can improve the overall experience in terms of surgical time, recovery, and outcome.
Certain preoperative medications greatly enhance the patient’s experience in controlling postoperative pain, as well as managing blood pressure throughout surgery and reducing postoperative nausea and vomiting.
All of my surgical patients, unless contraindications exist, receive 8 mg intravenously of Decadron, 0.1 mg p.o. of Clonidine, and 40 mg p.o. of Emend prior to surgery. This cocktail reduces inflammation and postoperative nausea, and improves hemodynamic stability throughout surgery.
Intraoperatively, a combination of Quill sutures and Insorb staplers speeds closure times markedly.
Quill sutures are PDS barbed sutures used for the SFS layer that distribute tension evenly across the closure. I use Insorb staplers for deep dermal closure, which provides good approximation in a fraction of the time required for interrupted sutures.
The use of indwelling catheters placed during surgery to deliver local anesthesia improves postoperative pain control. I prefer the Striker pain pump, as it has a button for patients to push to deliver a slightly greater amount of local anesthesia.
The opportunity for patients to play a part in pain control provides both psychological and physiological benefits. The device usually stays in for 3 days and can be removed by the patient.
Finally, as the major risk of this operation is deep vein thrombosis (DVT), we send patients home after all major surgeries with sequential compression devices.
The unit that I recommend, which is made by Kendall, is both small and portable and provides cost-effective, nondrug DVT prophylaxis. Patients keep these units for 1 day to several days, when the risk of DVT formation is highest.
POSTOPERATIVE CARE
Almost all of my postbariatric body-contouring procedures are performed on an outpatient basis.
We operate an American Association for Accreditation of Ambulatory Surgery-approved, level-C surgical facility that operates under the watchful eye of a board-certified anesthesiologist.
Following surgery, the patient recovers in our recovery suite for 1 to 2 hours. Milestones that indicate readiness for discharge include stable and normal blood pressure, normal heart rate, and adequate pain control.
I check on patients the first evening after surgery via phone and see them the next day. At the first postoperative visit, all dressings are removed to ensure a thorough examination of the surgical area.
I look for such things as a hematoma or seroma formation. During that appointment, patients are instructed again on drain care, diet, medication regimen, and activity. This is followed by a review of what to expect during the upcoming week.
The pain pump, if used, typically comes out on day 3. Drains come out based on output after surgery, most often around day 7.
At approximately 4 weeks after surgery, I introduce the use of Mepitac silicone scar sheets in order to optimize ultimate scar formation. Patients usually wear a compression garment for about 6 weeks.
To facilitate postsurgical care and monitor patient progress, routine follow-up visits are conducted at 1 week, 2 weeks, and 4 weeks after surgery.
Additional examinations are scheduled for the 4-month and 1-year procedure anniversaries. This is, of course, if everything goes as expected. Patients are welcome to come to my office at any point for assistance, should there be complications following surgery.
Postoperative photos are usually taken at 4 months or 1 year after surgery. My patients receive copies of their before-and-after photos—they can remember how far they’ve come. In addition, the photos can serve to encourage them to continue their commitment to maintain their beautiful “new” body.
 |
 |
 |
| Figure 3. The anterior scar should dive less inferiorly and be a little flatter than in the female counterpart. In the posterior region, a flatter scar is best, as opposed to the scar I typically give female patients. | ||
SURGICAL TREATMENT STRATEGIES
Weight-loss patients probably embody the concept of individuality more than any other group of surgical patients. And massive weight loss can create profound changes in a person’s body.
For some post–weight-loss patients, a near normal appearance may be the result; but more often, excess skin and diet-resistant fat persists throughout the body.
Tailoring a surgical treatment plan to the needs of the individual is the art of successful body contouring. The surgeon and the patient must work together to best determine the treatment areas and the appropriate treatment sequence.
Patients must understand that this series of operations involves a trade of one problem for another: replacing excess skin and fat with scars.
In most cases, it’s a very fair trade; however, for some people the decision needs to be weighed carefully.
I approach body-contouring patients with the partnership concept in mind, striving to plan the sequence of procedures the patient desires, keeping in mind the principle of designing a safe and reasonable process.
I encourage the typical patient—one who requires the treatment of the central body, chest, arms, and legs—to have midbody surgery first. The lower-body lift is the best operation for many women who lose substantial amounts of weight.
For men, however, abdominoplasty with posterior flank liposuction is often a good alternative.
|
See also “More Than Just Skin Deep,” by Wendy Lewis, in the August 2007 issue of PSP. |
Whichever procedure is used for the central body, I prefer to perform it first as it affects, to some extent, other regions of the body.
In the male patient, the preoperative discussion focuses on how much the waist should be tightened and where to place the scar. I usually aim for a horizontal scar placement and abdominal plication that is not quite as tight as what I do for women.
The anterior scar should dive less inferiorly and be a little flatter than in the female counterpart. In the posterior region, a flatter scar is best, as opposed to the scar I typically give female patients—it resembles the upper half of a heart shape (which better circumscribes their gluteal region).
As many men are sensitive to the concept of aesthetic surgery and are concerned with privacy, it is important to keep the posterior scars on men low.
Much more often than women, men are apt to wear shorts and go without shirts … and they aren’t eager to call attention to their surgery. Therefore, I believe it is important to lift and defat the suprapubic area, to create the best aesthetic result in the peripubic region.
At the time of the body lift, I also perform medial thigh liposuction to get this area to contract as much as possible, especially in patients who are considering medial thigh lifts in the future.
As a second operation, I address the arms and chest. Arm surgery for men is similar to the procedure for women, with two options for scar placement.
Due to larger male muscle development, placing the incision in the bicipital groove is often the best option because there is a better likelihood of camouflaging the scar. The alternative placement is on the posterior portion of the upper arm.
Whereas I frequently offer this as an option, no patient has accepted it. Posterior placement results in a “racing scar” effect when the patient’s arms are at his sides—a choice men view as unacceptable.
I believe that carrying the incision through the axilla and down onto the chest wall is important. Axillary access mandates placement of a Z-plasty in the axilla to limit web formation during arm abduction.
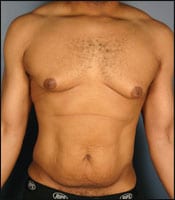
The male chest may be treated with either liposuction alone; circumareolar lift; or more aggressive procedures, such as inflammatory fold excision with free nipple grafting or nipple relocation based on the pedicle. The ultimate decision depends on the degree of deformity and how much residual tissue is present.
I usually finish treatment with a medial thigh lift. I use a T-shaped scar to achieve the greatest amount of skin resection and optimal scar placement. Although this operation usually involves one of the most challenging recoveries, it consistently makes patients happy.
 |
 |
| Figure 4. In the chest, significant weight loss can result in minimal deformity to significant gynecomastia. The approaches to treatment vary according to the degree of residual tissue and nipple ptosis. | |
CONCLUSION
As long as obesity continues to be an epidemic in the United States, I expect the number of patients seeking bariatric surgery and body contouring procedures will continue to climb.
Compared with women, men represent a relatively small percentage of patients seeking plastic surgery after weight loss. However, a significant number of them require care.
Optimizing their care necessitates judicious planning, precise operative technique, and meticulous postoperative attention to detail.
David S. Kaufman, MD, FACS, is a board-certified plastic surgeon in private practice in the Sacramento, Calif, area. He is a former Navy SEAL and graduate of Harvard Medical School. He specializes in plastic surgery for the massive weight loss community.