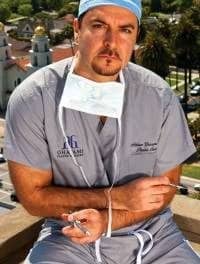
By Jeffrey Epstein, MD, and Gorana Kuka, MD
By Jeffrey Epstein, MD, and Gorana Kuka, MD
Hair loss is not just a man’s problem; women also experience it. Fully 40% of women have visible hair loss by the time they reach 40, and this increases after menopause. It is not easy for any woman to face changes that affect the quality and especially the quantity of her hair. For these reasons, hair loss in women can be devastating for self-confidence, self-image, and emotional well-being. Therefore, it shouldn’t be ignored. Successful treatment is possible as long as there is a differential diagnosis of the cause or causes.
Potential Causes of Female Hair Loss
When treating a woman with hair loss, do not merely attribute the loss to androgenetic alopecia (AGA), which is also known as male- and female-pattern baldness. Genetically inherited, AGA comes from either the mother’s or father’s side of the family or both, and results from androgens binding to the appropriate receptors on the genetically susceptible hair follicles.
This hormone-receptor complex activates the genes responsible for the gradual transformation of large “terminal” follicles to miniaturized “vellus” follicles. The result is a shorter cycle of hair growth for thinner strands of hair, and a delay in growth of new hair to replace strands that are shed.
In our experience, most cases of AGA in women are complicated by contributing factors that accelerate the process. These factors include but are not limited to: anemia, illness, medications, nutritional issues (including those associated with significant weight loss), hypothyroidism, Vitamin D deficiency, and more.
Some other contributing factors including post-childbirth or major illness cause telogen effluvium, which is the increased shedding of hairs 4 to 6 months after the inciting event due to a large percentage of the scalp hairs suddenly shifting from the “growing” anagen phase to the shedding telogen phase. Typically, telogen effluvium will reverse several months later, but when partnered with AGA, the hair loss may be permanent.
Hair loss is generally classified as non-scarring or scarring alopecia. AGA is the most common type of non-scarring alopecia, while others, including alopecia areata, telogen effluvium, anagen effluvium, and trichotillomania, are all characterized by a lack of destruction of the hair follicles.
Alopecia areata (AA) is an autoimmune inflammatory skin disease that causes hair loss on the scalp, beard, eyebrows, eyelashes, and other parts of the body. Typically starting with one or a few round patches of hair loss, it can progress to total scalp hair loss (alopecia totalis) and hair loss across the entire body (alopecia universalis), or just involve the eyebrows or other facial areas.
Diagnosis is made via history, exam (are there hairless patches or large alopecic areas in normal-appearing skin? or “exclamation mark” appearance of the hairs?), trichoscopy, and biopsy that is interpreted by an experienced dermatopathologist. Treatment consists of intralesional steroid injections and/or the induction of contact allergy, with inconsistent response rates. Fortunately, there is a high rate of spontaneous remission.
Hair transplantation is contraindicated in most cases of AA due the potential for recurrence. In our practice, we will transplant those areas that have been inactive (thus suggesting a “burning out” of the process), but even then patients are advised that long-term hair growth cannot be guaranteed.
There are a large number of types of scarring alopecia. While fortunately quite uncommon, they include lichen planopilaris, frontal fibrosing alopecia, central centrifugal alopecia (a common cause of crown hair loss in African women), folliculitis decalvans, and others which are all considered primary scarring alopecia because the hair follicle is the primary focus of the inflammatory process.
The secondary scarring alopecias include those due to traction and trauma (surgery, burns, accident). Hair transplant surgeons must be able to recognize when hair loss in a female patient is not simply AGA, as most of the primary scarring alopecias and the other non-scarring alopecia are not properly treated with hair transplantation.
The savvy surgeon should recognize something unusual in the hair loss, perform a biopsy or refer to a dermatologist, and most importantly not perform a hair transplant procedure that will most likely fail.
Matching Treatment to Diagnosis
Most female hair-loss patients are best treated with one or more of the following therapies:
• Treatment of the underlying medical condition(s).
• Medications. Rogaine (minoxidil, now in 5% approved for women once daily), spironolactone, and injections of steroids are options. We have not found finasteride to be effective in women.
• Laser light therapy. Done at home using a cap-like device, lasers yield an approximate 70% response rate in women with AGA.
• Platelet rich plasma (PRP) treatment. Injections of PRP may help reverse female hair loss.
• Nutritional approaches. Changes to the diet focused on restoring vitamin and protein deficiencies may also address some underlying causes of female hair loss.
• Hair-restoration procedures.
Focus on Female Hair Transplantation
The two techniques for transplanting hairs—follicular unit grafting (FUG) and follicular unit extraction (FUE)—differ only in the method of obtaining grafts. The rest of the procedure (recipient-site formation and graft placement) is the same. Both techniques are appropriate for women, with most choosing FUG because the typically fine line donor strip scar will not be visible unless the hair in the back of the head is shaved or cut very short. This is becoming an increasingly common way of treating women.
Hair transplantation is indicated for a variety of conditions. For example, thinning areas of female-pattern hair loss (FPHL) can be effectively filled in with procedures of between 800 and 1,800 grafts. With the commonly seen diffuse miniaturization that can occur in FPHL, there is a risk of “shock” hair loss to the existing hairs, and special precautions need to be taken by the surgeon that can help reduce the incidence.
Whether the high hairline is inherited, the result of receding due to AGA, or from a browlift or other prior plastic surgery procedure, it can be brought forward with the transplanting of hundreds to thousands of grafts.
The alternative to hair grafting for an overly high hairline is the surgical hairline advancement procedure. In this 90-minute procedure usually performed under oral sedation and local anesthesia, a patient with a sufficiently mobile scalp can have her hairline advanced by as much as 5 cm, with the ability to do simultaneous hair grafting into the upper temporal regions to help round out the hairline.
Hair transplants can be used to restore sideburns that were lost as the result of a previous facelift. A single procedure where typically 250 to 300 grafts can be transplanted into each sideburn can make a significant cosmetic improvement.
Hair grafting into the eyebrows can be an extremely effective way to restore eyebrows that are missing due to inheritance, overzealous plucking, laser hair removal or electrolysis, compulsive pulling, or the inadvertent result of prior surgery or permanent makeup gone awry.
These are delicate procedures that require the transplanting of as many as 350 grafts into each eyebrow via carefully crafted recipient sites that assure that the hairs will grow in the natural direction and pattern. Eyelashes can also be restored, and as with transplanted eyebrows, the hairs need to be trimmed on a monthly or bimonthly basis.
Caring for women with hair loss requires knowledge of proper hair transplantation techniques. Also critical, however, is recognizing when a patient is best treated by other approaches. This requires familiarity with the various pathologies that can affect women and their hair.
Jeffrey Epstein, MD, FACS, and Gorana Kuka, MD, are the directors of The Women’s Center for Hair Loss, with offices in Miami and NYC. They can be reached via [email protected].