
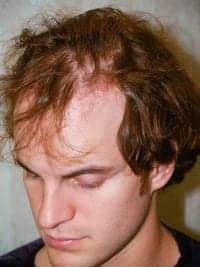
Donor area 1 day after FUE procedure.

Same donor area 6 months later.
For 18 years, I have specialized in surgical hair restoration, which makes up approximately 75% of my facial plastic surgery practice. This translates into performing more than 750 hair procedures annually. The majority are performed for male and female pattern hair loss, but there are also a variety of more specialized indications. These include eyebrow and beard restoration, hairline advancement (both with hair grafting as well as the surgical hairline advancement procedure), and many reparative procedures.
Since 1999, follicular unit grafting (FUG) has been the primary technique utilized in my practice for obtaining grafts. The FUG technique is labor intensive, requiring the individual microscopic dissection followed by transplanting as many as 3,000 or more grafts in a single procedure. Each of these grafts consist of a single follicular unit of one to three (occasionally four) hairs. To carry out these procedures, I employ 19 hair transplant technicians.
These technicians perform repetitive, but delicate work. They assist in the donor strip removal, dissect each graft, and then place each graft into the specific recipient sites one at a time. I create every recipient site because of the aesthetic importance in determining the distribution, pattern, and angulation of growth.
Another invaluable role all these technicians play is that of hostess/host. They greet, entertain, and befriend the patient who is often nervous before the 5- to 8-hour procedure.
ALL ABOUT FUE
As an alternative to FUG, the follicular unit extraction (FUE) technique avoids making a single donor-site incision. Instead, each graft, consisting of a single follicular unit like with FUG, is harvested one at a time via tiny punches. In my practice, these punches are usually 0.8 mm to 1.0 mm in diameter. Once extracted, these grafts can be trimmed of excess tissue under the microscope and placed into recipient sites. The donor sites, which can number as many as 2,000 or more in a single procedure, are allowed to heal. They usually result in undetectable dots that can permit patients to shave their head.

Before FUG procedure.

Twelve weeks after FUG procedure (3,200 grafts).
Before FUE procedure.

Twelve weeks after FUE procedure (2,100 grafts).
Since 2008, the FUE technique has been a regular part of my practice. It currently constitutes approximately 25% of the hair procedures I perform. It is particularly indicated in male patients who are less than 28 years old and thus at higher risk of donor scar widening, African Americans, and/or those individuals who wish to be able to shave their head.
There seems to be a consensus among my more experienced peers that FUE grafts, at least given current techniques, have a lower percentage of regrowth than FUG grafts, 75% to 80% versus 90% plus, respectively. In addition, FUE procedures require shaving of the back and/or sides of the head, can take longer to perform, and seem to ultimately provide a lower number of total grafts available for transplanting during a patient’s lifetime. Despite these challenges, FUE is a wonderful procedure for the right indications, and with developments in automation, these challenges may be further reduced.
ENTER ROBOTICS
Over the past 15 years, a variety of devices designed to automate the hair transplant procedure have been introduced. The first generation of these from the late 1990s to early 2000s included a “whacker” that cut hundreds of grafts in minutes using a guillotine-like device, a carousel implanter, and a pneumatic graft handler and placer. All three were intended to reduce surgical time and to replace the need for hair technicians during FUG procedures.
The automation devices introduced in the past 5 years have been designed for the FUE procedure. The earlier ones consisted of handheld drills to help with the extraction of grafts, but the more recent ones are more complicated, including the just-released ARTAS® System and NeoGraft®. While many consider these two similar, they have differences in what they are designed to do. That said, neither can provide artistic know-how or clinical judgment.
The ARTAS is a computer-assisted system that uses image guidance to determine which grafts to extract. It uses a two-step process. Once extracted by the ARTAS System, the grafts are transplanted by the surgeon and his technicians as they are with any other technique of hair transplantation. Currently there are few surgeons experienced with the ARTAS, but this number is sure to grow. It is believed by the company that ARTAS will likely follow the path of laser vision correction in that the new robotic technology will encourage more patients to undergo a hair transplant, creating vertical growth for FUE and an expansion of the total market for hair transplantation.


Twelve weeks after FUG procedure (3,200 grafts).
While I have less firsthand experience with NeoGraft, this device, under the control of the surgeon or technician, extracts then places grafts into recipient sites using pneumatic pressure to speed up the process of FUE. While originally promoted to hair transplant surgeons, the NeoGraft is now marketed directly to plastic surgeons, dermatologists, and other cosmetic doctors. These two devices are commendable for their advanced automation and technical aspects, and have the potential to advance the field of hair transplantation. They are particularly useful, at this time, for doctors who do not have a team of surgical assistants as they reduce the manpower needed to properly perform the procedure.
These devices do not replace the role of the surgeon in the treatment of hair loss. They do not make clinical judgments, nor evaluate the patient for the candidacy. Much like when addressing any other cosmetic concern, this knowledge comes through study, training, and experience. Age, etiology of hair loss, medical treatment, future permanence of donor hairs, and sex all help determine the best mode of treatment. Second, these automated devices do not replace aesthetic decision-making. Hairline position, design, and pattern, graft angulation and density, density of graft placement, distribution of grafts, and which areas to restore are all critical steps in the hair transplant process.
As a facial plastic surgeon, I view surgical hair restoration as a truly aesthetic procedure, and it can be as rewarding as any other cosmetic surgery for both patient and doctor. We as plastic surgeons have the opportunity to benefit from advancements in automation technology. These advancements are sure to become more and more common in the near future. We have a responsibility to our patients and our reputations to be sure that these advancements are embraced for the proper reasons, and continue to be our tools, not our replacements.
Fast Facts about Hair and Hair Transplantation
- Individuals lose 40 to 100 hairs each day due to the growth cycle of the hair follicle.
- The average person has 100,000 hairs on his/her head at any one time.
- More than 50 million men and about 21 million women in the United States are affected by hair loss.
- More than 40% of men will experience noticeable hair loss by age 35.
- 65% of women will have noticeable hair loss by age 60.
- More than 100,000 hair transplant surgeries were performed in the United States in 2010.
- There were 279,381 hair transplants performed worldwide in 2010.
Sources: International Society of Hair Restoration Surgery, American Academy of Facial Plastic and Reconstructive Surgery
Jeffrey S. Epstein, MD, FACS, is the director of the Foundation for Hair Restoration, and maintains full-time offices in Miami and New York City. He is also a Voluntary Assistant Professor at the University of Miami. He can be reached at [email protected].




