Call him the dermal filler king. Steven F. Weiner, MD, a board-certified plastic surgeon and owner of the Aesthetic Clinique in Santa Rosa Beach, Fla, currently ranks as the No.1 physician trainer for dermatological company Galderma and saw his practice earn “Best Medical Spa in the United States” honors at The Aesthetic Show in 2018. Below, he shares his best practices when injecting dermal fillers.
Plastic Surgery Practice: What trends or developments in aesthetics are driving new patients into your office?
Steven F. Weiner, MD: Interest in fillers, neuromodulators, lasers, and body contouring are driving new patients into my practice. Most important to patients is having minimal downtime, minimal risks, and natural results.
PSP: Are you seeing an uptick in interest in dermal fillers from certain patient groups?
Weiner: We are seeing an increase in interest from all age groups. Probably the most significant change is among younger patients, 30 and below, who are starting treatments for enhancement or correcting facial features they are unhappy with.
PSP: What concerns do first-time patients have (ie, too much filler (pillow face), filler mitigation, etc), and how do you address these concerns?
Weiner: First-time patients want to be comfortable and confident that the procedure they are receiving is safe. We assure patients that safety is our highest priority. These safety measures include cannula use for injections, which is safer than needles. (A recent study showed a roughly 75% less chance of vascular occlusion when cannulas were used versus needles.) Our office utilizes the most advanced injection techniques to minimize swelling, bruising, and to maximize safety.
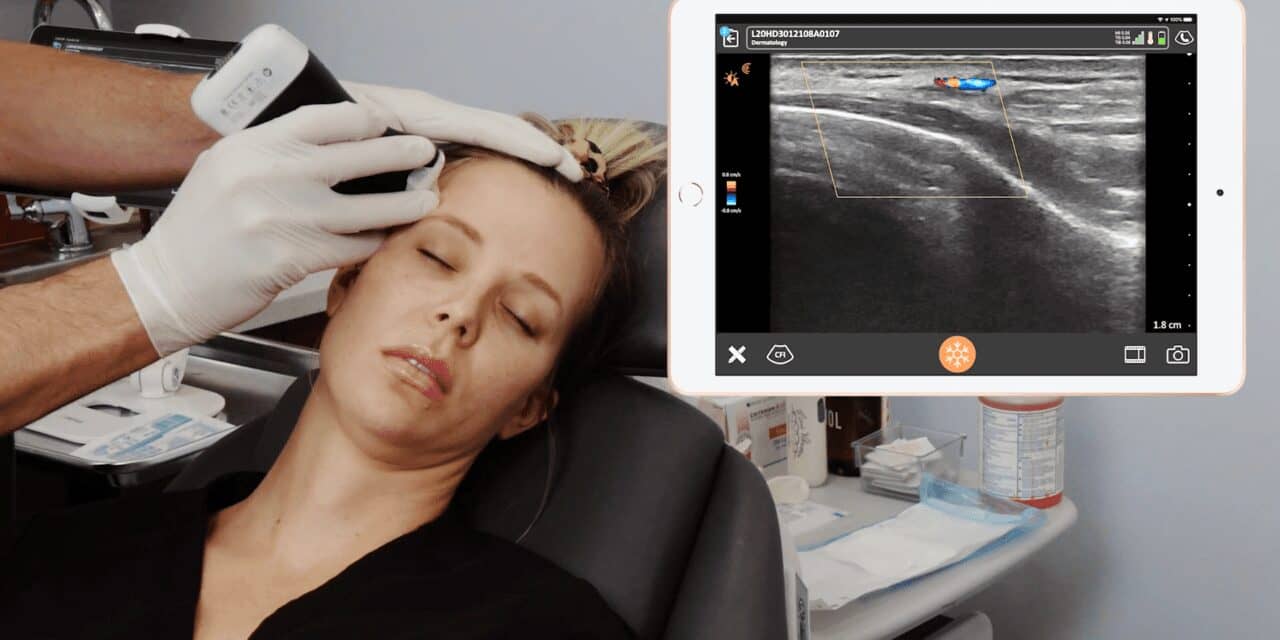
We also incorporate facial ultrasound, such as the Clarius L20, to evaluate facial anatomy and vascularity, and the presence, location, and composition of previously placed fillers. We show ‘befores’ and ‘afters’ of patients and have staff members explain the procedures they’ve had—all with natural-appearing results.
PSP: What steps do you take to put patients, including new patients, at ease in advance of a filler treatment?
Weiner: Patients feel reassured by my credentials and my staff’s credentials. These include surgical training at Johns Hopkins Hospital, monthly courses on facial ultrasound and anatomy, trainings throughout the United States, published works, including peer-reviewed industry papers, and participation in several FDA clinical trials. I have dedicated my career to achieving optimal and safe filler results and have trained physicians all over the world on my filler techniques.
PSP: Are there techniques you incorporate or products you like to use with first-time patients or with patients who have had a bad experience with fillers in the past?
Weiner: We use cannulas to improve safety and minimize swelling, bruising, and discomfort. If requested, we can incorporate “ProNox”, which is nitrous oxide, or laughing gas, to make patients more comfortable. If they are concerned about vascular complications, high-frequency ultrasound, the Clarius L20, can be used to vascularly map the face to identify the location and depth of critical arteries. Knowing vascular location can reduce the chances of having a vascular occlusion, a rare but serious complication from filler injections.
PSP: Can you provide an example of a challenging filler case and share your approach?
Weiner: A patient comes in with swelling around their eyes and wants improvement of their “eye bags.” When asked about prior filler in the cheek or tear trough, the patient shares that they had filler about eight to 10 years ago, “so it’s all gone by now.” Being skeptical, I used the Clarius L20 to evaluate the lower eyelid. Filler (hyaluronic acid) was found in the area of swelling, and the filler was dissolved using hyaluronidase. The patient’s eyebags were resolved in a couple days, with a very simple procedure.
PSP: Are there any new tools available to help minimize risks and ensure better results with fillers?
Weiner: Using microcannulas and ultrasound is considered state-of-the-art techniques to minimize risk and ensure best results. Cannulas are less likely to enter a vascular structure when compared to a needle and thereby have less risk of bruising and occlusions. Ultrasound enables the injector to determine the anatomy of the patient sitting in your chair, because anatomy, particularly vascular anatomy, is inherently variable. Mapping the vascular structures in critical areas such as the temple, nose, pyriform, and chin will limit the risk of having a vascular occlusion. PSP