|
Most cosmetic surgeons that were not “injection oriented” a decade ago now realize that fillers and neurotoxins have become an integral and necessary part of contemporary cosmetic surgery.
All fillers are capable of causing complications and most complications occur proximal to the syringe, meaning they are the fault of the surgeon or injector. When discussing filler-related complications, one must differentiate sequelae from true complications. Swelling and redness are sequelae; and hematoma, overfill, or granuloma are complications.
Some of the more commonly seen filler “complications” include the following:
- Swelling;
- Bruising;
- Asymmetric fill;
- Overcorrection;
- Tyndall Effect (superficial injection);
- Hematoma; and,
- Herpetic flare.
NO PAIN, LOTS OF GAIN
Although pain control may seem out of place in an article about filler complications, I believe it is extremely relevant. One thing that has always amazed and bothered me is the cavalier attitude that many injectors take when it comes to pain control with filler injection. One of the best ways to get a grip on this concept is to get filler injections yourself, which usually makes most injectors think differently on the subject
Injecting a numb patient is a better experience for both the surgeon and patient, and a more precise procedure can be performed when pain is removed from the experience.
I always shake my head when I hear an experienced injector say, “My patients are tough; they don’t need pain control.” These are the type of doctors I want doing business down the street, because sooner or later I will get their patients. I can’t tell you how many filler patients that have come to my office, who have repeatedly had filler injection in other practices and then became my permanent patients because my procedure was painless.
They best way for a surgeon to understand this concept is to think about the dental model. Many people judge their dentist not by competence but by the comfort level of the visit.
Most physicians assume that because they can inject the nasolabial fold without local anesthesia, that anesthesia is not necessary. Wrong. If rethought, the entire process can be made painless.
For facial cutaneous filler injection, I first mark the patient and apply a BLT-type topical anesthetic (20% benzocaine, 6% lidocaine, and 4% tetracaine) on the skin. BLT topical anesthesia can be compounded by most local pharmacies. Then I use a 1 cc syringe with a 32-gauge needle and inject lateral and deep to the nasolabial fold as to not distort the area to be filled. By placing 0.05 cc’s of 2% lidocaine with 1:100,000 epinephrine in two to three areas from the nasal base to the lips, the remainder of the procedure will be 100% painless. Trust me when I say my patients are appreciative and loyal when I do this.
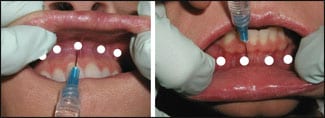 |
| Figure 1. The injection points for the “mini block” technique—0.2 cc’s of local anesthesia injected in the perisulcular region, from the canine tooth one side to the canine tooth on the other side in each jaw. |
 |
| Figure 2. In this example of overtreatment an area of filler that has been overfilled is extruded after puncture with an 18-gauge needle. |
For lip injections, I use a “mini block” technique that I have published in the past.1 As soon as the patient arrives at the office, the lips are wiped with alcohol and marked with a surgical marker. A thin coat of BLT topical anesthesia is applied to the inside of the lips (and sulcus) and the vermillion. After 5 minutes, I perform four to five injections of the aforementioned local anesthetic just above the sulcus in the upper lip and just below the sulcus in the lower lip.
It is important to use a 1 cc syringe and a 32-gauge needle, as the injection mechanics and pain perception are minimal with this setup. I inject 0.1 cc into several areas from the canine tooth on one side to the canine tooth on the other side (Figure 1).
At this point, I apply ice to the lips; after 5 minutes, the patient is ready for painless lip augmentation. I am not an advocate of nerve blocks, as they leave the patient with an entirely numb face when they leave—patients do not appreciate this. In addition, as the frequency of “missed” blocks is high, infiltrations always work. Immediately postinjection, ice is reapplied.
My approach has a few drawbacks. First, it takes a bit longer than most procedures; however, in the long run this pays off exponentially. Second, when patients are anesthetized by the mini-block technique the lip movement will frequently be affected; therefore, the patient must be marked before the injections so that the landmarks are not lost by the decrease in perioral motor function.
Regardless of these minor drawbacks, a pain-free procedure benefits both surgeon and patient.
FOLLOWING UP INCREASES MARKETING AND PROTECTS YOUR REPUTATION
One of the most important factors in dealing with filler complications is to first recognize them. Although this may sound trivial, many physicians do not routinely follow up with their filler patients. Scheduling a follow-up appointment for all filler patients allows you to review the results. Even the most accomplished injectors will encounter patients who may require some touching up.
Too many physicians assume that if a patient does not call back to complain about something, then the result is acceptable. In reality, it may be acceptable to the patient who does not understand the nuances of a great result; however, it may undermine the surgeon’s reputation in the patient’s eyes.
I call my filler patients 2 weeks post-treatment and, although I think I am a very experienced injector, I still find some patients with good results that can be made better. One very important thing to keep in mind is what I call the filler marketing factor—every patient becomes a walking and talking advertisement for you and your practice.
Patients may not appreciate the finer points of a good result. For instance, if a patient is walking around with under-correction or lumps and bumps, it reflects on your reputation. If you don’t bring the patient back for follow-up appointment, you simply won’t know.
From a marketing standpoint, every time you get a patient to return to your office for any reason, you can make positive marketing impressions. And the more they come to your office, the more they bond with you as their surgeon—plain and simple.
TREATING COMPLICATIONS
Irregular fill. When patients see me after working with another physician, the most common complication is “lumpy” fill, which can be prevented by judicious massage by the injector at the time of treatment. My assistant keeps a small dollop of Vaseline on the back of her glove, which I continually use to coat the patient’s skin or lips and massage during and immediately after the injection. This simple method will obtain a homogenous fill and prevent visible and palpable lumps.
 |
| Figure 3. Patient shown with excess filler in the tear trough regions 24 hours after hyaluronidase injection. |
Undertreatment. This is a common complication, in part due to the cost of fillers. Many patients attempt to gain “unrealistic mileage” from a single syringe of filler. We have all had the patient who presents with the desire to purchase a single syringe and wants multiple areas treated. Another clue to this syndrome is when a preinjection consultation begins with the patient saying “… and if you have any filler left over …”
Patient expectations must be clarified in terms of filler coverage. I refuse to inject the nasolabial folds of most adults with a single syringe of filler because most adults will obtain a suboptimal result—more material is needed. Trying to please them with a single syringe has too often ended with an unhappy patient because the result was subpar. Trying to be the “good guy” will sometimes make you out to be a villain, which equates to negative marketing. “Save your money and return when you can afford two syringes,” is what I tell the patient with unrealistic expectations.
Another common cause of undertreatment, especially for the novice injector, is injecting too deeply when treating the skin, wrinkles, and folds. Most of the common fillers are meant for intradermal injection and, if injected into the subcutaneous plane, they lateralize instead of plump. When I teach filler injections, I stress that if you can’t see the wrinkle of fold improve as you inject, you are too deep.
Overtreatment. Underfilling is pretty easy to deal with: Add more filler. However, overtreatment presents additional challenges.
The first consideration is the nature of the filler. Permanent fillers—such as silicone oil, Artefill, or even autogenous fat—can be very challenging to remove or reduce. Long-lasting fillers such as Radiesse or Evolence can also present challenges in the area of removal or reduction.
The hyaluronic acid fillers, though, have an inherent “insurance policy,” as they can be quickly and easily reversed with hyaluronidase.
When a patient presents with an overfilled area, conservative treatment should be employed. Sometimes, regardless of the filler, simply having the patient manually massage the overfilled area in the direction of the normal side can reduce the area of excess. Another way to deal with excess filler is to make a puncture over the area of excess and attempt to extrude it (Figure 2).
As stated earlier, a big advantage of using hyaluronic acid fillers is the fact that they can be quickly, easily, and safely reversed. Hyaluronidase is an enzyme that hydrolyzes hyaluronic acid. The action is rapid and occurs in several hours to several days.
When the need to reverse a hyaluronic acid filler presents, the hyaluronidase must be injected at the level of the filler. When reversing a hyaluronic filler in the tear trough (nasojugal groove) region, the hyaluronidase must be injected at the periosteal level and/or any area of fill.
Similarly, when reversing a treatment given to the skin or lips, the hyaluronidase must be deposited in any area that contains the filler.
Hyaluronidase can be purchased in 1 cc vials containing 150 units of hyaluronic acid. I mix this with 1 cc of local anesthesia or saline, which yields 2 cc’s of 75 units each.
When I want to reverse all the filler, I inject 75 units in the tissue plane containing the filler. This would include one side of a tear trough (nasojugal fold), one nasolabial fold, or a single lip. If I want to reduce but not eliminate the total filler volume, I inject about 15 units for a subtotal reduction. This enzyme will also dissolve some of the native hyaluronic acid in the skin, which is quickly replenished. I tell patients that the treated area may look puckered for several days but will return to normal.
Tyndall Effect. The Tyndall Effect is an illusion of color that is produced. When clear hyaluronic acid gel is injected too superficially under the thin lower eyelid skin, it can appear blue (Figure 3).
Blue light is more strongly scattered than red light—the same effect that causes the sky and ocean to look blue. This can also be demonstrated by dissolving white flour in clear water, which creates a blue color.
Although some authors debate this effect with fillers, there is no doubt it occurs. The effect can be reversed via hyaluronidase injection (Figure 4).
EVERSING NON-HYALURONIC ACID FILLERS
 |
| Figure 4. This patient is shown after hyaluronic acid injection in the periorbital regions, which produced a bluish hue under the eyes. She is shown 48 hours after filler dissolution using 75 units of hyaluronidase in each lower-lid region. |
Although not as readily predictable as hyaluronidase, other fillers can sometimes be reduced by the injection of triamcinolone or betamethasone into the overfilled region.
Intralesional steroids have been shown to decrease collagen and glycosaminoglycan production via their anti-inflammatory properties.2 Steroids have also been shown to decrease the proliferation of fibroblasts and are also thought to be associated with a decrease in plasma protease inhibitors, allowing for an increase in collagenase activity.3
In addition, there have been studies of the reversal of Evolence (porcine collagen) in a laboratory model.4 Multiple, intentional areas of product accumulation were created by injecting 0.2 mL of Evolence intradermally into the backs of test animals. After 2 weeks, the injections were repeated. The areas were then evaluated histopathogically and analyzed histomorphometrically (height characteristics) after an additional 2 weeks.
After 4 weeks, saline was injected in the control sites, and 0.25 mg/0.1 mg bethamethasone diproprionate/betamethasone phosphate or 2 mg methylprednisolone was injected into the test locations.
At the conclusion of the analysis, it was evident that the injection of either steroid directly into the areas of product accumulation led to a decreased height and presentation of Evolence collagen within the dermis.
As new collagen fillers such as Evolence reach the United States, the concept of reversal with collagenase would be very welcomed. Currently, commercial collagenase is not available in America.
Xiaflex is a collagenase enzyme for intralesional injection for the treatment of Dupuytren’s contracture, Peyronie’s disease, and Frozen Shoulder syndrome (Adhesive Capsulitis). Clinical trials for this and other uses are currently under way. If this drug becomes available and is effective in dissolving collagen, overfill complications from Evolence and other collagen fillers may be treated just as we use hyaluronidase for hyaluronic acid reversal.
CONCLUSION
The number of filler options, longevity, and predictability of these products has improved dramatically over the last decade. As with most procedures, complications can result. Both the treating surgeon and patient must be aware of these common complications, as well as their avoidance and treatment options.
Joseph Niamtu III, DMD, is a board-certified oral and maxillofacial surgeon in private practice in Richmond, Va. He can be reached at .
REFERENCES
- Niamtu J. Simple technique for lip and nasolabial fold anesthesia for injectable fillers. Dermatol Surg. 2005;31:1330-1332
- Manufacturer and User Facility Device Experience Database. Available at: www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfMAUDE/search.cfm. Accessed August 11, 2009.
- Niessen FB, Spauwen PHM, Schalkwijk J, Kon M. On the nature of hypertrophic scars and keloids: a review. Plast Reconstr Surg. 1999;104(5):1435-1458.
- Nir E, Goldlust A. Steroidal treatment of Evolence and Evolence Breeze in an intracutaneous model in rat (Study Number: PC10). Data on file, ColBar LifeScience Ltd, 2009.
OVERSEAS UPDATE: 70 FILLERS OF CHOICE
It is difficult to believe that just 10 years ago most US surgeons had but two choices for injectable fillers: bovine collagen and bovine collagen. Although Zyplast and Zyderm could produce acceptable augmentation and were easy to use and teach, the longevity of the products was simply not acceptable.
Today’s surgeons outside of the United States have an almost incomprehensible array of filler options. Many of my European colleagues have access to around 70 choices of approved fillers in their countries, though most injectors use only a small fraction of these.
Looking at the history of filler progress in this country, the biggest changes occurred with the introduction of the non-animal stabilized hyaluronic acid (NASHA) fillers, such as Restylane and Perlane, Juvéderm Ultra and Ultra Plus, Captique, Elevess, and Prevel Silk.
Due to their predictability, ease of injection, and longevity, the filler landscape changed almost overnight. In addition, these fillers (in part to their hydrophilic properties) did not require overcorrection—injectors had to rethink their injection techniques.
The NASHA fillers remain the most popular treatment options among US injectors. It is now common for patients to main results predictably for 6 to 12 months.
The quest for longer-lasting injectable materials was, in effect, prior to the introduction of NASHA fillers in this country. Although on the surface the term “permanent filler” sounds like the perfect option, I remind my patients that permanent fillers can cause permanent complications. Any busy injector has more than once whispered to their assistant, “I’ll be glad when that dissolves.”
A hydroxylapatite filler, such as Radiesse, is an option for a longer-lasting result, but in my opinion it is not an option for the lips. Polymethlymethacrylate spheres, as in Artefill, seemed to be a good permanent option for dermal injection, but suspended in a bovine collagen matrix it was a throwback from the past and the company that made Artefill went out of business in America.
Silicone oil (Silikon 1000) has been a “permanent” filler option for a half of a century and constitutes a significant portion of my injectable practice. Love it or hate it, this option is quite predictable but very technique-sensitive.
As the waves of the Atlantic continue to wash up new fillers from abroad, we have seen a new porcine collagen filler, Evolence, which does not require allergy testing and has gotten the attention of many surgeons for its smooth injection properties and longevity.
As these products continue to be used outside the United States, many of them will also make their way through the FDA.
As far as complications, we have been warned by our overseas colleagues about filler-associated complications. Severe granulomatous reactions and a host of other problems have been well-reported abroad and will sooner or later become journal fodder in this country as well.
—JN