|
Women and surgeons have become more aware of the nonmedical genital effects of childbirth, weight fluctuations, tissue laxity, and anatomic idiosyncrasies—all of which can be addressed by a variety of procedures.
Knowledge of the nomenclature, the functional pelvic floor anatomy, and the patient’s specific concerns is the key to establishing a successful surgical plan.
Not infrequently, patients will present with both a cosmetic request and a legitimate medical complaint. In such situations, it is critical to conduct a full gynecologic and/or urologic assessment. Failure to do so may result in patient dissatisfaction with the cosmetic procedure or, worse, aggravation of the medical problem.
In many instances, the therapeutic and cosmetic surgeries can be performed under the same anesthesia. Furthermore, the patient and the physician must always keep in mind and discuss the potential effects of the cosmetic procedure on future vaginal childbirth. Along those lines, a future cesarean delivery by patient request may not always be available.
Although cosmetic vaginal surgery is the general term, three commonly treated areas are actually external or vulvar structures. These include the mons pubis, the labia majora, and the labia minora, which also include the clitoral hood or prepuce.
The perineum, the bridge of tissue between the anus and the vagina, and the lower third of the posterior vaginal wall are typically the target areas of vaginal tightening procedures.
The anterior vaginal wall plays a lesser role in vaginal tightening but a far greater role in the surgical treatment of urinary incontinence. The remnants of the hymen typically are reconstructed when a request is made for cultural reasons.
Anesthesia for vaginal surgery can be general, epidural, spinal, or intravenous sedation with local block. I favor the latter and most commonly employ a propofol drip monitored by an anesthesiologist.
The local anesthetic is a modification of the traditional pudendal block, employing approximately 60 cc of tumescent lidocaine per side and a low-volume infiltration of the surgical site with the same solution.
Prophylactic antibiotics are routinely employed for vaginal surgery, and, typically, I administer intravenous ceftriaxone 500 mg or doxycycline 100 mg prior to surgery.
Patients are positioned in dorsal lithotomy, with the legs supported in boot-type stirrups with mild flexion of the knee. Intermittent pneumatic compression stockings are routinely employed. Indwelling bladder catheterization is employed during most operations. Bladder catheterization is maintained postoperatively for 24 hours in cases in which periurethral swelling is anticipated and when vaginal packing is placed.
MONS PUBIS
Two classes of procedures are performed on the mons pubis—liposuction and lifting.
Liposuction is the most common cosmetic treatment for this area and is typically performed in the supine position at the time of general abdominal liposuction.
I prefer to use 2.5- and 3-mm cannulas for this region in order to deliberately slow the pace of fat removal and prevent overaggressive debulking irregularities.
The end point of mons pubis liposuction is an even thickness of the fat contours between the areas cephalad and caudad to the pubic bone, but without “skeletonizing” the latter. Mons pubis liposuction is also incorporated during abdominoplasty when the lower incision edge is thicker than the upper edge, and yields far more cosmetic contours along the central incision line.
The mons pubis lift is an effective aesthetic option for women with significant laxity in the mons pubis region and sagging of the labia majora as viewed in the standing position. It is achieved by carefully controlling the central tension vectors when planning the resection pattern at the time of abdominoplasty.
Whether or not the procedure is a lower abdomen-only mini procedure, a lipo-abdominoplasty, or a full abdominoplasty, there are two keys to achieving an optimal lift: avoid excess tension at the angles of the pubic triangle, and avoid curving the center of the scar cephalad.
These goals are best accomplished with a high lateral tension-style excision pattern. The pubic lift integrates well with mons pubis liposuction and yields a more complete and balanced aesthetic solution for the abdominal wall aesthetic unit.
 |
 |
| Figure 1A. Congenital unilateral hypertrophy of left labium minus, which produced traction pain and obvious asymmetry in a 22-year-old nullipara. | Figure 1B. Treatment consisted of left-sided reduction labia minoraplasty. The extent of resection extends from the fourchette to the posterior margin of the clitoral prepuce. |
THE CLITORAL REGION
Cosmetic alterations in this region are limited to the excision of loose, redundant folds of skin from the prepuce. It is essential to maintain symmetry while resecting and approximating these tissues to avoid deviating the alignment of the clitoral shaft away from the midline.
Due to the extremely sensitive innervation of this area and the relative thinness of the anatomy, minimal electrocautery—very superficial incisions and fine absorbable sutures such as 6-0 synthetic absorbable monofilament—is preferred. The surgeon should avoid placing incisions across the dorsum of the prepuce along the clitoral shaft because they will be visible when the patient is viewed in the standing position. Maintaining incision lines parallel to or within the natural skin folds produces an effective camouflage and is very difficult to detect even by an untrained eye.
When planning surgery of this type in combination with a mons pubis lift, the lift is done first because it frequently produces a tightening of the prepuce in the vertical axis when the mons pubis is placed on cephalad traction.
Inferior to the prepuce, the trifurcation of the posterolateral portion or the prepuce, the frenulum, and the labium minus poses a technical challenge when prepuce alterations and reduction of the labia minora are requested by the patient.
The best way to address the vectors necessary for both symmetry and a smooth appearance is to leave this area for the final stage of the combined procedure and split the inner from the outer surfaces of the labia minora. This achieves proper vectoring of traction forces without creating visible bunching of the outer surface. Each case presents unique considerations, and a full discussion is beyond the scope of this article.
 |
 |
| Figure 2A. Preoperative resection pattern marked on the perineum for vaginal tightening communicates with a similar-sized triangle of posterior vaginal epithelium marked internally (not shown) in a 36-year-old multipara. Superficial and deep tissues are approximated in the midline to achieve tightening. | Figure 2B. Immediate postoperative appearance following posterior vaginal tightening and augmentation of labia majora by autologous fat transfer of 30 cc of purified fat per side via anterior incisions. |
THE LABIA MINORA
In my practice, reduction labiaplasty of the labia minora is the second most often requested procedure after vaginal tightening.
The most common indication is patient dissatisfaction with elongated, asymmetric, or hyperpigmented labial tissue. The patient’s articulation of her exact complaint directs the extent of resection.
Occasionally, patients will request the repair of chronic torn labial tissue years after vaginal childbirth.
When examining the labia minora, it is necessary to splay them laterally onto the labia majora to determine the degrees of hypertrophy, hyperpigmentation, and asymmetry that may be present. Excision lines are marked at this time and are demonstrated to the patient with a hand mirror.
When bilateral excisions are planned, both sides are approximated to match the excision lines. Anteriorly, the excision line may end inferior to, at, or beyond the clitoral frenulum. Posteriorly, the excision line may extend toward the fourchette in the midline.
When performing combined reduction labiaplasty and vaginal tightening procedures, vaginal tightening is performed first because it involves the resection of the fourchette, with subsequent reconstruction in a more anterior position. Laterally, resection should never encroach beyond the natural crease between the labium minus and the labium majus because it may produce gaping and expose the urethra.
Sutures at the edge of the labia minor are best applied with 5-0 braided synthetic absorbable material. Monofilament knot tails produce significant discomfort and should be avoided. Likewise, the placement of temporary permanent sutures is hampered by the significant patient discomfort experienced during removal.
Suture lines are dressed with Vaseline at the conclusion of surgery, and patients are instructed to wear boxer shorts for the first 2 weeks, to avoid inserting anything in the vagina for 6 weeks, and to avoid prolonged sitting on the suture lines for 6 weeks. Local edema and bruising are common in the first 2 weeks following these operations.
 |
| Figure 3. The folds of the clitoral prepuce normally extend posteriorly and fuse with the labia minora, as demonstrated in a 29-year-old multipara. The labia minora display mild hypertrophy and moderate hyperpigmentation, which were this patient’s cosmetic concern. Effective cosmetic reduction labia minoraplasty must include resection of excess skin from the lateral prepuce, and the suture lines must create a smooth-flowing surface from anterior to posterior. |
THE LABIA MAJORA
Three procedures are available for cosmetic alteration of the labia majora: autologous fat transfer, resection of loose skin, and sclerotherapy.
The labia majora frequently lose volume with age and weight loss, producing a deflated appearance with looseness and wrinkling of the overlying skin. In most patients, these changes can be addressed effectively with autologous fat transfer.
Similar to fat grafting in facial applications, you harvest a sufficient amount of fat from a suitable site, prepared according to your preferred technique; you then inject it into the subcutaneous fat layer.
Anesthesia is limited to a bilateral pudendal block and a low-volume infiltration of tumescent lidocaine, as described above. Approximately 20 to 30 mL of purified fat are injected subcutaneous in a fanlike pattern through bilateral anterior stab incisions using a 15-cm-long, 14-gauge Coleman Type 2 blunt cannula. Deep injections should be avoided, as they may disrupt the structures of the vestibule. Postoperative edema and bruising are the rule and are managed expectantly. I try to avoid cold packs in order to maximize blood flow to the transplanted fat cells.
Autologous fat transfer will not produce a tight appearance of the labia majora when a greater degree of skin laxity and sagging is present, usually in massive-weight-loss patients. In addition, larger-volume fat grafting does not yield a desirable effect.
In these situations, an ellipsoid full-thickness skin resection in the long axis of the labia majora—either alone or in conjunction with autologous fat transfer—will provide an effective cosmetic solution.
The anesthesia is the same type that is used for fat grafting. Suture lines are closed in two layers using a 5-0 synthetic absorbable suture—a subcutaneous layer of interrupted stitches and an intradermal layer of running suture, followed by an application of topical skin adhesive.
Varicose veins of the vulvar region respond to sclerotherapy in much the same manner as those of the lower extremity. Not infrequently, these varicosities are a source of pelvic pain. A gynecologic workup for pain should rule out other etiologies prior to treatment.
Sodium tetradecyl sulfate 1% is my preferred sclerosing agent; it is administered via 32-gauge needles attached to tuberculin syringes. Five 1-mL injections per side are given in a typical session using sterile technique. The veins are targeted in the standing position and injected in the supine position. The technique is identical to sclerotherapy of the leg varicosities, working from proximal to distal veins. A pelvic compression garment is worn for the first 7 days.
 |
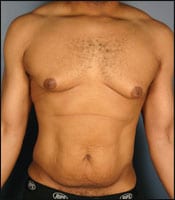
| Figure 4. Significant pathology, visible in a 48-year-old multipara who is unsuitable for standard vaginal tightening, includes (anterior to posterior) cystocele with stress urinary incontinence, rectocele, and attenuation of the perineum. Treatment includes bilateral paravaginal bladder suspension, transobturator synthetic sling, vaginal hysterectomy, culdeplasty, site-specific rectocele repair, and perineoplasty. |
VAGINAL TIGHTENING
Commonly known as vaginal rejuvenation, procedures for tightening the vaginal caliber are derivations and variations of a class of gynecologic operations referred to as vaginoplasties or colporrhapies.
In therapeutic gynecologic surgery, these operations are among those used for the treatment of prolapse of the bladder (cystocele) and of the posterior vaginal wall (rectocele), although they have been largely replaced by more anatomic, site-specific procedures—and with the advent of reliable synthetic mesh.
Nonetheless, in the absence of advanced degrees of pelvic organ prolapse, mild to moderate degrees of vaginal laxity can be corrected quite adequately by targeting the lower third of the posterior vaginal wall and the perineal body for plication.
I do not recommend performing these operations on the anterior vaginal wall because they do not add significant tightening at the sites most commonly noted by patients as loose. In addition, they have proven to have a high failure rate for their intended effects in therapeutic gynecologic surgery.
Experience with the management of complex pelvic surgical conditions is mandatory for surgeons embarking upon vaginal tightening procedures, due to the frequency with which anatomic distortion from childbirth-related scarring is encountered in this region, and also because of the proximity to the bladder and rectum.
In addition, gauging the degree of tightening can be tricky in experienced hands, and those considering offering these surgeries to their patients are well advised to seek specific training in these operations from experts.
CONCLUSION
A variety of procedures are available for the enhancement of the female genitalia. Despite controversy, they continue to grow in popularity. Familiarity with the array of aesthetic options delineated above permits the cosmetic surgeon to make a realistic assessment of the ways in which the female patient’s concerns may be addressed. Many of these procedures are within the skill sets of seasoned cosmetic surgeons. For more complex procedures, however, establishing a successful treatment plan may necessitate collaboration with an experienced pelvic surgeon.
Marco A. Pelosi III, MD, FACOG, FACS, FICS, FAACS, is the chairman of obstetrics and gynecology of the International College of Surgeons and founder of the International Society of Cosmetogynecology. He can be reached at www.iscgyn.com or .