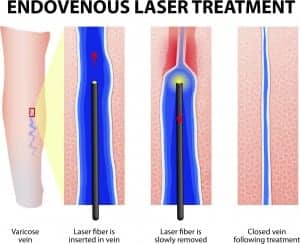
A new study comparing three treatments for varicose veins suggests that when it comes to quality of life improvements, all three are equal.
The study, which appears in the September 25, 2014 issue of The New England Journal of Medicine, compared endovenous laser ablation, foam scletotherapy, and surgery among 798 patients with primary varicose veins at 11 centers in the UK. The study’s primary end points were disease-specific quality of life and overall quality of life at 6 months. Secondary outcomes included complications and measures of clinical success.
The mean disease-specific quality of life was slightly worse after treatment with foam sclerotherapy than surgery, but similar among patients in the laser and surgery groups. There were no differences in quality of life seen among patients in any of the groups following treatment. That said, one-third of the participants in the laser group received foam sclerotherapy at 6 weeks for residual varicosities, which may have affected quality of life rating.
Complication rates, including lumpiness, staining, and numbness, were lower after laser treatment than after foam or surgery, the study showed. The frequency of serious adverse events was about 3% in all groups. Clinical success measures were also similar among groups, but successful ablation of the main trunk of the saphenous vein was less common in the foam group than in the surgery or laser group.
“The differences were small, and we can’t generalize the finding to every patient,” says Natalie Evans, MD, a vascular medicine specialist at Cleveland Clinic in Ohio. Importantly, study participants were deemed candidates for all three procedures before randomization, she says. In clinical practice, not all patients would be appropriate candidates for sclerotherapy.
“This is not a death knell for sclerotherapy,” she says. “A reputable doctor will make a decision on what is best for the patient. There isn’t a cookie cutter or algorithm,” she tells Plastic Surgery Practice.
Foam Sclerotherapy Comes of Age
Varithena, by BTG, became commercially available in August 2014 after receiving approval from the US Food and Drug Administration in late 2013. This treatment combines Polidocanol and a carbon dioxide mix to create new injectable foam. It can be used to treat veins in the great saphenous vein system, which runs the entire length of the leg.
“Foam treatments have come a long way,” says Mitchel P. Goldman, MD, American Society for Dermatologic Surgery (ASDS) president and co-founder of Cosmetic Laser Dermatology in San Diego. Goldman disussed the treatment of varicose veins at a recent media conference sponsored by the ASDS in New York City. He conducted clinical trials on Varithena before the FDA approval.
A survey of 221 patients who participated in the final clinical trial for Varithena shows success with the new treatment, Goldman says. At 1 year post-treatment, the patients showed consistent improvements in appearance, disease severity, and symptoms such as heaviness, aching, swelling, throbbing, and itching. “I have no doubt Varithena will be an important addition for physicians’ abilities to treat leg veins successfully,” he says.