Applying some of the principles of craniofacial surgery can help maximize patient outcomes after facial transplantation, according to an article in The Journal of Craniofacial Surgery.
In patients with extensive facial defects including loss of the normal bone and soft tissue landmarks, a “reverse craniofacial planning” approach can restore normal facial relationships, according to researchers led by Edward J. Caterson, MD, a member of the facial transplant team at Brigham and Women’s Hospital/Harvard Medical School in Boston.
Caterson and colleagues apply some basic principles of craniofacial surgery to the planning and performance of facial transplants. Most patients who are candidates for facial transplant have loss of soft tissues only. However, some also have defects of the underlying facial bones. In these cases, the challenge for the facial transplant team is nothing less than “the complete restoration of the structural anatomy of the craniofacial skeleton,” they write.
Craniofacial surgeons have developed an understanding of the “intimate functional relationship” between the facial soft tissue and supporting bone. In the traditional craniofacial procedure, the surgeon carefully plans and designs “bone movements that will translate into a desired change of the attached soft tissues.” But in facial transplantation, the situation is essentially reversed: The degree of injury and the subsequent transplantation of facial soft tissues dictate the “osteosynthesis” of the craniofacial skeleton.
A Simple, Practical Technique
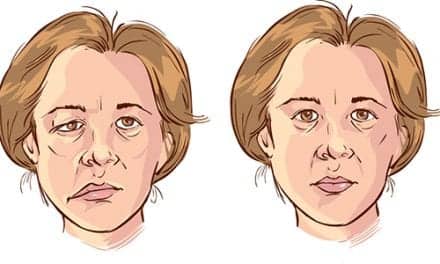
In the new study, Caterson and colleagues describe a simple but practical technique for surgical planning to promote proper positioning of the facial transplant. The technique applies “normative” data on facial landmarks and relationships and then transposes them onto the recipient.
Optimal positioning of the facial transplant is essential not only to achieve the most normal-appearing result, but also to maximize function