 |
| Figure 1. Injecting several areas across the maxillary or mandibular sulcus area will provide adequate local anesthesia without distorting the area to be injected. Preinjection topical will make the injections much more tolerable. |
Is injectable fillers are the most commonly requested procedures in our industry, the term “aesthetic surgery” may have become a misnomer. Even for those of us who cut and sew every day, nonsurgical aesthetic treatment has become a huge part of our practices.
We have gone from using a single injectable filler to becoming “bartenders” of sorts, as patients come in requesting the filler du jour. The current options give surgeons latitude when choosing the best-quality product for the given aesthetic concern. I find myself using specific products for specific anatomic areas based on feel and longevity and, of course, what works best in my hands.
Though some fillers appear to have distinct advantages over others, many fillers conjure “Coke versus Pepsi” comparisons. Some are very forgiving while others warrant extreme conservatism. That said, the introduction of so-called “permanent” fillers will surely produce a wave of complications in our industry.
An experienced injector can probably use just about any filler effectively, whereas a novice injector is much more prone to producing lumps and bumps in unhappy patients.
I favor the hyalurons, as they can be used in almost any situation, although I also use hydroxyapatite, poly(l-lactic) acid, human collagen, silicone, and fat.
PREPARING THE PATIENT
 |
| Figure 2. The youthful lip has definition and pout. Senescent changes in the fat, muscle, and skin cause a lengthening of the lip with loss of definition and volume. |
A considerate surgeon can control outcome and patient satisfaction by controlling the injection. Find out whether or not the patient is taking any medications or supplements that could affect coagulation and encourage bruising. Provide the patient with a list of common medications that affect platelet function; and ask them to refrain from such meds for 2 weeks, in order to lessen ecchymosis.
Surgeons will, at times, cause bruising; however, repeated or consistent bruising is eventually going to drive away patients. They trust us to make them look better, and if you let them leave your office with purple lips, then they may not come back.
I prefer to ice patients both before and after the procedure. With patients who are prone to bruising, I will substitute a blunt microfat injection cannula for the normal beveled needle.
It is essential that you develop a reputation for being a pain-free injector. There is no doubt that proper preinjection pain management takes longer and is more hassle for the surgeon and staff. However, it is paramount that the patient remains comfortable at all times.
To that end, although many options exist, topical anesthesia followed by local injection provides the best pain control.
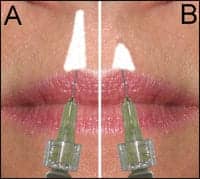
 |
| Figure 3. Injecting the vermilion/cutaneous junction to create a youthful white roll requires depositing the filler in the correct plane. Injecting in the potential space beneath the lip mucosa should allow free antegrade and retrograde flow with minor syringe pressure (3A). Lack of free flow or lumping with increased syringe pressure means the needle is improperly positioned (3B). |
I use a topical anesthetic of Betacaine 20%, Lidocaine 6%, and Tetracaine 4%, mixed at the local pharmacy, for profound topical anesthesia. When you arrive at the patient’s face, thoroughly wipe off all lipstick, makeup, and skin oil before applying anesthetic.
In general, most patients need only topical anesthesia for cutaneous injections, such as nasolabial folds. Although many injectors use infraorbital or mental nerve blocks, I would rather not see my patients walk around for several hours with a totally numb face. I prefer local infiltrations that dissipate more quickly.
For lip injection, the topical anesthesia is applied using a Q-tip swab in the upper and/or lower sulcus. After around 5 minutes, local anesthesia (2% Lidocaine with 1:100,000 epinephrine) is injected in the upper and/or lower gingival sulcus. Approximately 1/4 cc to 1/2 cc is injected just above the sulcus in the upper lip and just below the sulcus in the lower lip, in four to five areas, using a 32-gauge needle (Figure 1).
This process will usually supply adequate local anesthesia that should result in a painless injection procedure.
For those patients who cannot tolerate nasolabial fold injection, 1 cc of the same solution can be injected through the skin (after the topical) in the deeper tissues of the nasolabial fold. It is important to use small amounts of local and to inject deeply, so as not to distort the fold prior to injection. Anesthesia is especially important near the nostrils, where the injections are often painful.
TREATING THE LIPS AND PERIORAL AREAS
 |
| Figure 4. This patient was treated with 1.5 cc’s of a hyaluronic acid filler by providing definition and pout. |
This is the most commonly requested filler treatment in my practice. As each patient presents with a different set of problems, there is no common or single treatment for this area.
The younger the patient, the easier he or she is to treat—they often require only simple volume. The senescent lip offers the biggest challenge, with multiple potential problems, including loss of outline, loss of volume, perioral vertical rhytids, deep nasolabial folds, and “marionette lines.” In addition, the senescent lip is elongated due to atrophic factors, actinic damage, and the loss of tooth structure (Figure 2).
Several important factors must be addressed, especially for the novice injector. First and foremost is the need to be conservative in your approach to these procedures.
All too often, we characterize filler injection as a “wham bam” single treatment procedure (eg, botulinum toxin Type A) when, in reality, filler injection is a sculpting process.
During the consultation, I tell patients that I am sculpting their anatomy, which may require more than a single treatment in order to achieve the best aesthetic result.
In this manner, I can provide a more conservative initial treatment. Also, the patient should be comfortable with returning for a touch-up, if necessary.
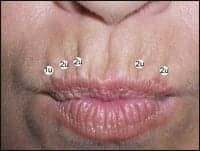
 |
| Figure 5. Treating the philtral columns is an integral part of lip rejuvenation. Younger patients can frequently be treated by minor triangular filler injection at the base of the philtrum (5A). Older patients frequently require enhancement of the entire philtral column (5B). |
Therefore, it is extremely important for you to meet with your patients after the initial treatment, for numerous reasons. The number one reason? To evaluate the results. Although the patient may be pleased with the outcome, I may observe, say, an asymmetry or other fault that could reflect on the quality of my work.
For the younger patient, simple volume injection is all that is usually required. This is performed by depositing the filler at the wet/dry line, one third to one half of the thickness of the lip (for deep plumping). Although some injectors prefer to inject while advancing, I prefer to inject while withdrawing the needle.
Most patients only need augmentation of the central one-third of the upper and lower lips, or what I call the “pucker” area. A surprising small amount of filler in each lip will create a pleasing pout in most patients with youthful lips.
In most patients, it is not necessary to extend the injection laterally all the way to the commissures. In fact, I try to avoid this as it produces a “ducky” look and screams of overtreatment.
In patients who are older or have lost natural lip contours, outline definition is important in addition to plumping. Defining the “white roll” of Cupid’s bow in the upper lip and the cutaneous/vermillion junction of the lower lip restores youthful definition.
The correct tissue level of injection is in the potential space under the lip mucosa. When in the proper plane, the syringe pressure should be minimal and the filler should flow both antegrade and retrograde. If the syringe pressure is high or if the filler is not freely flowing, then the needle is not in the proper plane and it must be repositioned (Figure 3).
 |
| Figure 6. This image shows typical filler injection of upper and lower lip outline, volume, and philtral definition. |
For example, the patient shown in Figure 4 was treated with 1.5 cc’s of a hyaluronic acid filler used to restore outline and pout.
One of the most overlooked areas of lip enhancement is the philtral columns. In younger patients, only the inferior portion of the columns needs defining, whereas older patients may require definition from the nostril to the vermilion (Figure 5A). Simply depositing a small triangle of filler at the base of the columns can serve to enhance the result in most patients (Figure 5B).
A typical treatment sequence of injecting the philtral columns is depicted in Figure 6—both white roll and deep lip.
TREATING VERTICAL LIP RHYTIDS
This is a very challenging area. Although many patients ask to have the individual vertical lines injected separately, this can produce a series of “speed bumps” across the lips.
I prefer to enhance this area by simply adding lip volume and white roll definition, which in combination stretches the lip and improves the wrinkles.
 |
| Figure 7. A series of injections of one to two units of botulinum toxin Type A across the upper and lower lips can enhance the treatment of vertical rhytids as well as prolong increased longevity of the fillers. |
For those patients who refuse bigger lips, I favor human collagen for treating this area. The fluid viscosity of this filler allows
for rhytids improvement without a thickened appearance. Also, pretreat this area with botulinum toxin Type A and have the patient return in 1 week. Reducing the orbicularis tension can further improve the result of the filler.
Figure 7 shows the generalized areas of botulinum toxin Type A injection in a typical patient, and Figure 8 shows a before-and-after treatment that used both botulinum toxin Type A and human-derived collagen for vertical lip lines. Note that in both images the patient is puckering.
TREATING THE NASOLABIAL FOLDS
In my practice, the nasolabial folds represent the second-most-requested area for fillers. Experience has shown that the most frequent problem with treatment failures is an inadequate amount of fillers.
Many patients—especially first-timers—desire only a single syringe of filler, split equally in both folds. Although this may be adequate for younger patients, most adults with even moderately deep folds will require at least a full syringe in each fold.
 |
| Figure 8. This patient was pretreated with two units of botulinum toxin Type A in several areas of the upper and lower lips and injected a week later with filler. This treatment must remain conservative to not affect orbicularis function. |
In patients hesitant to make that investment, I encourage them to postpone treatment until they can afford two syringes.
One caveat: When injecting the nasolabial folds, do not make them deeper. Although this sounds unusual, I have seen numerous patients who were improperly injected elsewhere. The problem is that the nasolabial folds represent a junction of numerous soft tissue planes. If the filler is injected in the deepest valley of the fold, then it can flow laterally and actually make the fold bigger.
When teaching filler injection, I stress the fact that the injector should actually see the folds improve as he or she is injecting. Although this sounds simple, novice injectors sometimes do not appreciate this. When injecting in the fold, if it does not fill immediately then the filler may be flowing laterally. The injector needs to reposition the needle medial to the fold in order to redirect the filler. In this case, what you see is what you get.
 |
| See also “Rhinoplasty Minus the Knife” by Steven H. Dayan, MD, FACS, in the February 2007 issue of PSP. |
Another problem with inexperienced clinicians is depositing the filler too deeply. Most hyaluronic acid fillers are meant for intradermal injection. If they are injected subcutaneously, they will flow laterally instead of plumping the fold or wrinkle. If the fold or wrinkle is not improving before your eyes, the needle should be redirected into a more superficial plane.
Obviously, some fillers are intended for subcutaneous injection, but they are usually more robust in particle size and longevity. Knowing what filler to place in what area is key to successful and lasting outcomes.
Figure 9 shows a patient treated with approximately 1 cc of hyaluronic acid filler in each nasolabial fold and an additional 1 cc split between the perioral wrinkles and mentolabial fold.
 |
| Figure 9. This patient was treated with 1 cc of hyaluronic acid filler in each nasolabial fold. |
Joseph P. Niamtu III, DMD, is a board-certified oral and maxillofacial surgeon in private practice in Richmond, Va. He can be reached at [email protected].



