By Michael A. Fallucco, MD, and Ziv M. Peled, MD
As the surgical treatment of migraine headache evolves, plastic surgeons are learning that this modality actually represents a series of procedures designed to relieve pressure on specific peripheral nerves throughout the head and neck.
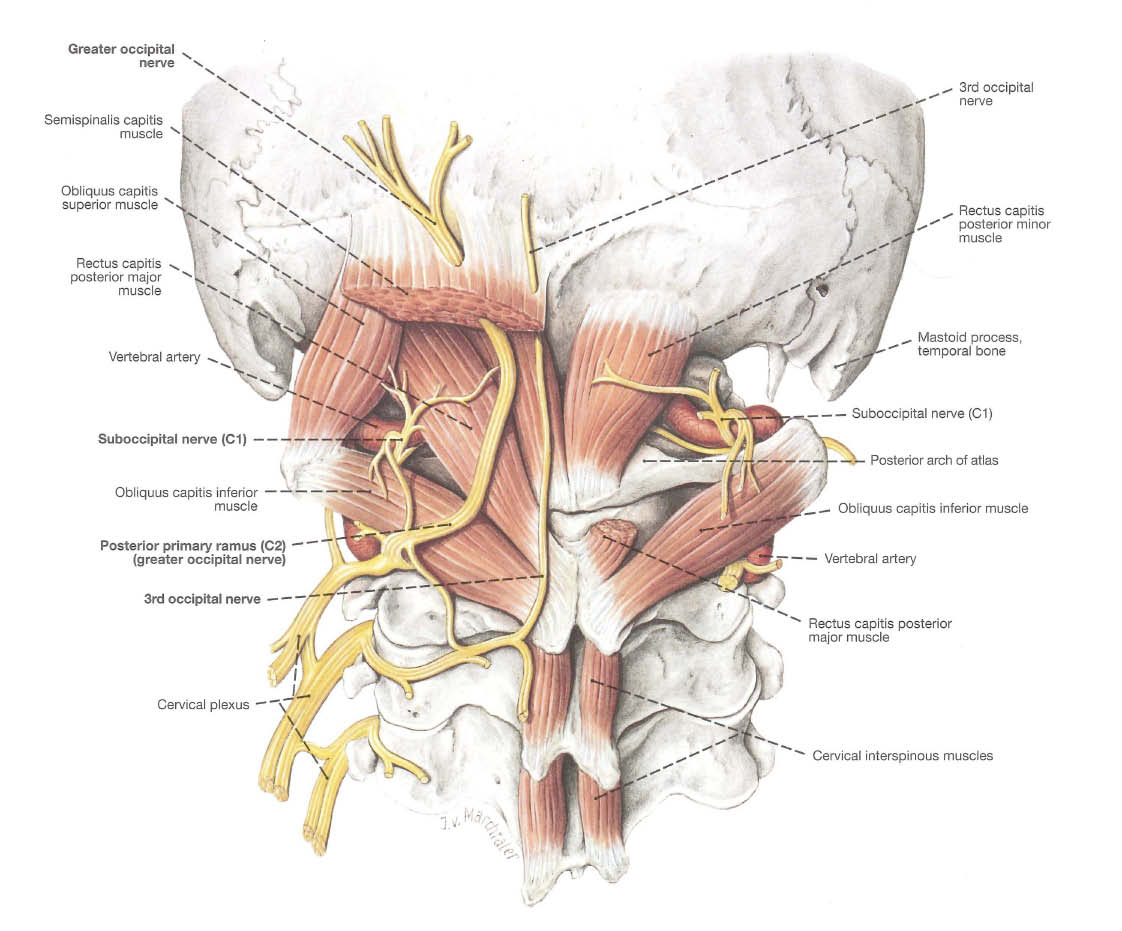
Occipital neuralgia or cervicalgia relates to occipital-generated headaches that stem from the greater (C2) and least (C3) occipital nerves. The occipital trigger sites are the most common trigger points of headache pain.
All patients presenting with chronic daily headaches should be evaluated by a neurologist or primary care physician who is familiar with International Headache Society guidelines for these disorders. Once this evaluation is complete, a thorough history focused on identifying peripheral nerve compression should be performed. The history should quantify the subjective complaints of pain by using the Migraine Disability Assessment Tool (MIDAS) or the migraine headache index (MHI). Once the severity of disability has been stratified, it is important to ask where the pain consistently starts and radiates, whether there is a history of trauma such as whiplash, and if there are any previous cervical surgery/pathology and/or any other issues specific to the occipital region.
 |
| Preop Occipital Decompression marking. |
CASE EXAMPLE
A 35-year-old otolaryngologist presents with a 4-year history of headache pain that originates at the posterior skull/neck junction and worse on the left side. Complete evaluation by his neurologist, including MRI/CT, was unremarkable. He complains of throbbing 8 out of 10 pain for more than 15 days per month, lasting 4 to 12 hours. The pain radiates to the temples and the back of his eyes. He does not wake up in the morning with a headache. Rather, the pain increases throughout the day. He has zero days out of the month without some pain. He was struck by an automobile 10 years prior to onset of headache pain. His MIDAS score is 150. A MIDAS of 21 or higher suggests severe disability.
He has severe tenderness to palpation from the paramedian nuchal ridge caudal to the C3 level. He denies any upper-extremity paresthesias or weakness.
X MARKS THE SPOT
We have isolated the occipital trigger site as the likely origin of pain and have eliminated other potential “red flag” causes for the symptoms. We prefer diagnostic, local anesthetic blocks over Botox chemodenervation in occipital trigger site verification for the greater occipital nerve (GON) and least
occipital nerves (LON). The local anesthetic block provides near immediate feedback. In our experience, Botox is difficult to titrate for the deep neck musculature.
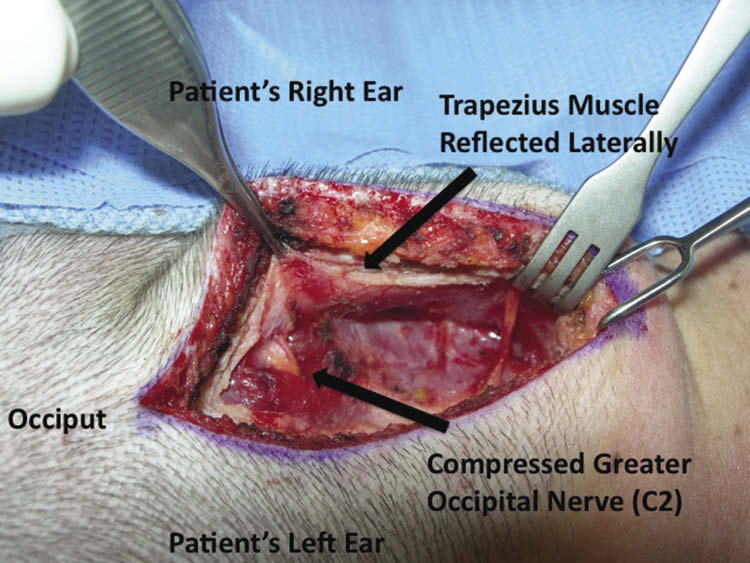 |
| Figure 1. Compressed Greater Occipital Nerve (C2). (Click to Enlarge) |
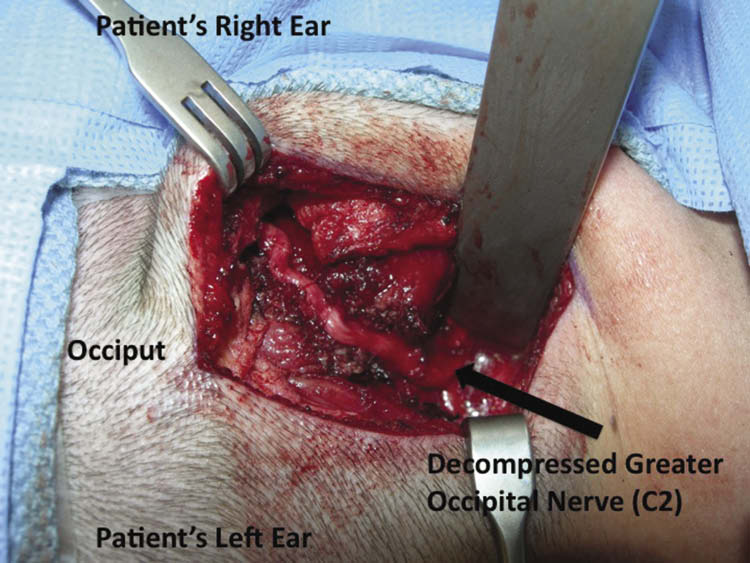 |
| Figure 2. Decompressed Greater Occipital Nerve (C2). (Click to Enlarge) |
We recommend local anesthetic with a 27-gauge needle for those first learning this identification technique. Safety is paramount, and frequent negative aspiration prior to injection and only injecting while moving the needle retrograde will decrease the risk of intravascular injection. The use of ultrasound or fluoroscopy is another aid for precise needle placement. If performed properly, a patient with ongoing pain from occipital nerve compression should experience near immediate reduction on their visual analogue pain scale. Lesser sources of pain, if present, may be verified at this time with step-wise blocks of the frontal and temporal trigger sites.
In the OR
|
Read Dr Falluco’s original article on surgical deactivation of the peripheral migraine trigger site: Headache Helper – Can Plastic Surgery Really Cure Migraine Headache? |
The patient should be in the prone position with slight neck flexion. Meticulous positioning must be verified to prevent postoperative complications due to excessive pressure. A midline is drawn from the occipital protuberance to the 7th cervical vertebra, and the upper portion within the hair follicles is used for incision. Dissection is carried down to the trapezius fascia, and the subcutaneous tissue is cleared from its superficial surface working laterally.
A paramedian incision through the trapezius fascia allows identification of the LON, which may be dissected caudal to its spinal origin for neurectomy or decompression. If LON neurectomy is performed, the GON location as it traverses the semispinalis muscle is first verified by reflecting the trapezius laterally (Figure 1). With the LON treated, the GON is now neurolyzed distally and superficially by releasing the trapezius muscle’s tendinous insertion at the nuchal line.
At this point, we prefer to cauterize the occipital artery/vein with bipolar electrocautery and are diligent to evaluate for and remove any enlarged lymph nodes that can occupy this already tight tunnel toward the temple. The GON distal release is now complete (Figure 2), and we work proximally and deeply, performing a partial semispinalis muscle resection, then releasing the investing fascia encircling the nerve down to the obliquus capitis inferioris muscle and even deeper to the last dense layer of fascia as the posterior ramus of C2 exits the spine.
Care must be taken at these deeper levels due to the large occipital veins that can easily make visualization difficult. The field is irrigated and anesthetized, and the entire extraspinal GON course is visualized to ensure no acute angles as it traverses the cervical musculature from deep to superficial. If acute angles are present, intramuscular transposition is performed. Lastly, the trapezius muscle which has been released distally is rotated and advanced to allow vascularized coverage of the GON at its distal, superficial, and vulnerable location near the nuchal line. The incision is closed, and no drains are utilized.
Results can be immediate, and headache relief is long-lasting. Typical recovery following occipital surgery involves rest for the first week, followed by a physical therapy program focusing on range-of-motion exercises. Patients will go through a period of paresthesias/dyesthesias for
1 to 2 months. These are treated with topical compounding agents for symptomatic relief. This operation, along with others that target different trigger sites, have dramatically improved the quality of life for migraineurs.
 |
 |
| Michael A. Fallucco, MD, (l) and Ziv M. Peled, MD, (r) are board-certified plastic surgeons in private practice in Jacksonville, Fla, and San Francisco. They can be reached via [email protected]. | |



